Operational Considerations for the Identification of Healthcare Workers and Inpatients with Suspected COVID-19 in non-US Healthcare Settings
Written by COVID-19 NEWS on February 21, 2021
The U.S. Centers for Disease Control and Prevention (CDC) is working closely with international partners to respond to the coronavirus disease 2019 (COVID-19) pandemic. CDC provides technical assistance to help other countries increase their ability to prevent, detect, and respond to health threats, including COVID-19.
This document is provided by CDC and is intended for use in non-US healthcare settings.
1. Overview
This document provides guidance on the identification or screening of healthcare workers1 and inpatients with symptoms of suspected COVID-19. Rational, requirements, and considerations will be discussed for three broad case identification strategies:
- Passive strategies: Reporting/alerts are initiated by the data source (e.g., healthcare worker or treating clinician) based on a known set of rules or regulations.
- Enhanced passive strategies: Reporting/alerts are initiated by the data source with an added mechanism to prompt data collection, review, and/or reporting.
- Active strategies: Reporting/alerts are initiated by the centralized health authority (e.g., Ministry of Health, facility infection preventionist, facility administration) using a known set of rules or regulations.
Additional guidance on managing visitors to healthcare facilities and triage of suspected COVID-19 patients in non-US healthcare settings is also available.
While, epidemiologic, virologic, and modeling reports support the possibility of SARS-CoV-2, the virus that causes COVID-19, transmission from persons who are presymptomatic (SARS-CoV-2 detected before symptom onset) or asymptomatic (SARS-CoV-2 detected but symptoms never develop), critical knowledge gaps remain regarding the benefit of routine or repeated screening of healthcare workers and inpatients without symptoms for prevention of COVID-19 spread within health facilities outside of an outbreak response scenario.2 Therefore, discussion around optimal testing strategies for the identification of healthcare workers with presymptomatic and asymptomatic SARS-CoV-2 infection are outside the scope of this guidance.
2. Signs and Symptoms Consistent with COVID-19
Presenting signs and symptoms of COVID-19 vary, limiting the definition of a generalizable set of characteristic signs and symptoms for COVID-19. At best, current evidence suggests substantial variability ranging from mild to severe and based on only partially described patient-level factors. The WHO interim guidance for clinical management of COVID-19external icon provides the following summary of published COVID-19 symptom descriptions and observed frequency (see box):
Among persons who develop symptoms, most experience fever (83%–99%), cough (59%–82%), fatigue (44%–70%), anorexia (40%–84%), shortness of breath (31%–40%), and myalgias (11%–35%). Other non-specific symptoms, such as sore throat, nasal congestion, headache, diarrhea, nausea, and vomiting, have also been reported. Loss of smell (anosmia) or loss of taste (ageusia) preceding the onset of respiratory symptoms has also been reported.
Older people and immunosuppressed patients in particular may present with atypical symptoms such as fatigue, reduced alertness, reduced mobility, diarrhea, loss of appetite, delirium, and absence of fever.
Symptoms such as dyspnea, fever, gastrointestinal (GI) symptoms or fatigue due to physiologic adaptations in pregnant women, adverse pregnancy events, or other diseases such as malaria, may overlap with symptoms of COVID-19.
Children might not have reported fever or cough as frequently as adults.
Given these limitations, facilities should define a standardized set of signs and symptoms (e.g., fever and/or cough/shortness of breath) to screen healthcare workers and patients for suspected COVID-19. A high level of suspicion is critical to ensure cases do not go unrecognized due to a substantial proportion of patients and healthcare workers presenting with atypical or minimal symptoms.
3. General Best Practices
In addition to a specific strategy for the identification of suspected COVID-19 cases, there are general best practices that will improve both healthcare worker and inpatient COVID-19 screening. Some examples include:
Monitor and Manage Ill and Exposed Healthcare Workers
- Facilities and organizations providing healthcare should implement sick leave policies for healthcare workers that are non-punitive, flexible, and consistent with public health guidance.
- Movement and monitoring decisions for healthcare workers with exposure to COVID-19 should be made in consultation with public health authorities.
Train and Educate Healthcare Workers
- Provide healthcare workers with job- or task-specific education and training on identifying and preventing transmission of infectious agents, including refresher training.
- Ensure that healthcare workers are educated, trained, and have practiced the appropriate use of personal protective equipment (PPE) prior to caring for a patient.
- Provide job-aids and up-to-date reference materials.
- Encourage and support a high index of suspicion in healthcare workers regarding suspect COVID-19 cases.
Establish Reporting within and between Healthcare Facilities and to Public Health Authorities
- Implement mechanisms and policies that promote situational awareness for facility staff about confirmed or suspected COVID-19 patients and facility plans for response, including:
- Infection control
- Healthcare epidemiology
- Facility leadership
- Occupational health
- Clinical laboratory
- Frontline staff
- Communicate and collaborate with public health authorities.
- Communicate information about confirmed or suspected COVID-19 patients to appropriate personnel before transferring to other departments in the facility and to other healthcare facilities.
4. Surveillance Capacities
Facility-based surveillance for healthcare-associated infections (HAIs), including infections in healthcare workers and inpatients, is one of the WHO’s eight core components of infection prevention and control (IPC)external icon. While surveillance is a critical component of providing safe healthcare, it is important to recognize that it requires expertise, good quality data, and an established IPC program and thus, may require time to set up. For this reason, during public health emergency response, healthcare facilities are encouraged to initially implement facility-based, suspect COVID-19 patient case finding (surveillance) that is feasible with existing surveillance capacities.
Health facility surveillance capacity varies greatly even within health systems. A realistic appraisal of capacity can help identify the best strategy for a given context. A general description of surveillance capacities based on existing HAI surveillance activity is provided for guidance.
5. Identification of Healthcare workers with suspected COVID-19
Objective: Prevent exposure of at-risk patients and staff to symptomatic COVID-19 positive healthcare workers.
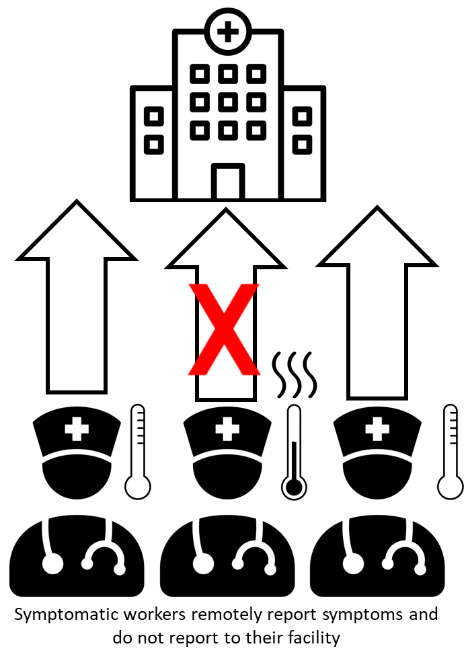
Figure: Passive identification of healthcare workers with suspected COVID-19
Passive strategy
All healthcare workers self-assess for fever and/or a defined set of newly present symptoms indicative of COVID-19. If fever or respiratory symptoms are present, healthcare workers:
- Remotely report this information4
- Do not go to their health facility
- Are provided with immediate medical assessment and follow-up actions
Rationale:
Establishes mechanisms for the identification of healthcare workers at increased likelihood of infection with minimal resource requirements.
Requirements:
- List of symptoms and thermometer for self-assessment.
- Staff and mechanism (e.g., telephone line) for remote reporting of fever and/or presence of symptoms consistent with COVID-19. Ideally this system is always available for quick medical assessment. If reporting system is not available, symptomatic healthcare workers should not report to their facility until they can be evaluated.
- Decision algorithms for response to healthcare worker reports and the results of secondary assessment.
- Standardized medical assessment and movement and monitoring forms.
Considerations:
- Adherence is highly dependent on healthcare worker motivation and appropriate self-assessment of risk.
- Can result in reduction in work force, particularly among some critical staffing categories.
- Provision of paid sick leave/compensation for all healthcare workers not allowed to work is often critical for success, requiring substantial resources.
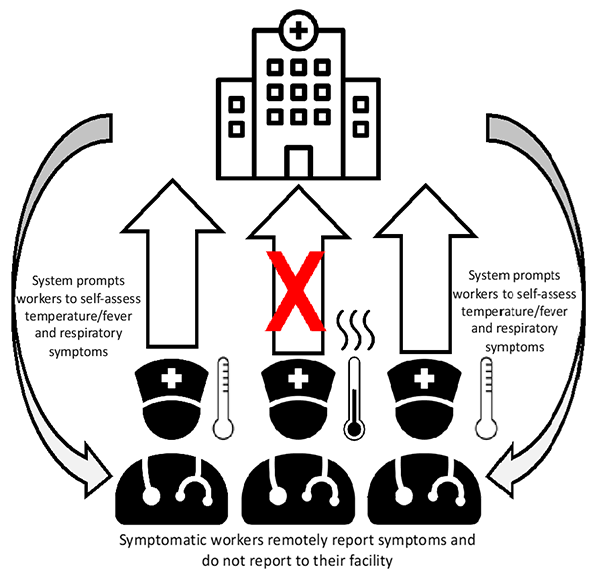
Figure: Enhanced passive identification of healthcare workers with suspected COVID-19
Enhanced passive strategy
In addition to passive strategy, establish a plan to remind or prompt workers to self-assess for symptoms consistent with COVID-19. Common reminders include automated text messages or phone calls.
Rationale:
Evidence suggests that simple automatic reminders can increase adherence.
Requirements:
- All requirements of Passive Strategy
- Automated (e.g., mass texting service) or manual system (e.g., direct messaging or phone calls) to contact healthcare workers as prompt for self-assessment
Requirements (Automated System):
- Mass Text Messaging Services capable of sending text messages to groups of people simultaneously. Mass Text Messaging Services are sometimes provided by independent internet-based service companies or are sometimes provided by cellular service providers.
- Database of contacts (i.e., healthcare workers under monitoring). In addition to contact number, database fields may include name, position, work unit/area, and monitoring end date.
- An effective and informative text message including frequency of messaging, timing of delivery, and any interactivity of interventions5.
Requirements (Manual System):
- Database of contacts (i.e., healthcare workers under monitoring). Because of the effort required in manual systems, this database should be carefully targeted to minimize workload and maximize benefit. Considerations for targeting might include:
- Documented COVID-19 exposure
- Serving a population at high-risk for severe illness from COVID-19
- Serving a population at increased risk of being COVID-19 positive cases
- Staff available to contact monitored healthcare workers with reminders.
- Phone and phone credit to support messaging and or calls.
Considerations:
- Same as Passive Strategy
- Funding may be required to support bulk text messaging
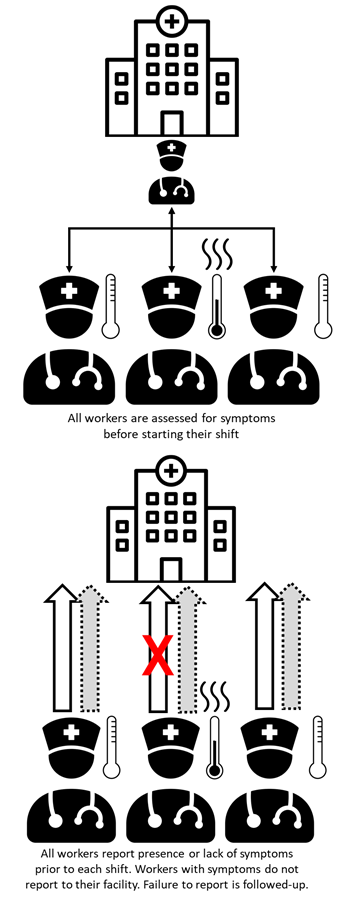
Figure: Active identification of healthcare workers with suspected COVID-19
Active strategy
All healthcare workers present for in-person evaluation of symptoms and fever prior to each shift. If symptoms consistent of COVID-19 are reported or observed, healthcare workers are provided with immediate follow-up actions.
Remote active strategy
All healthcare workers report (e.g., by call or text) the absence or presence of symptoms consistent with COVID-19 remotely each day. Staff that fail to report or report symptoms are followed up.
Rationale:
While there is limited evidence for the benefit of active healthcare worker monitoring, active strategies will theoretically result in increased healthcare worker adherence to self-evaluation of symptoms, thus enhancing patient and healthcare worker protection.
Requirements (Active strategy):
- All requirements of Passive Strategy
- Dedicated staff to evaluate healthcare workers before their shift (active) or respond and monitor healthcare worker reports
- Physical area for staff evaluations that will allow recommended social distancing (i.e., at least one meter according to WHO recommendations (CDC recommendation is at least 6 feet (1.8 meters)) and includes adequate hand hygiene stations (soap and running water or alcohol-based hand rub)
- No touch thermometers
- Implementation plan that includes a method to ensure that staff present at a given place for pre-shift evaluation
- Accountability system to ensure all healthcare workers have been evaluated (e.g., work slip sign-off)
Requirements (Remote Active Strategy):
- All requirements of Passive Strategy
- Accountability system to ensure all healthcare workers report in remotely prior to their work shift
Considerations:
- Same as Passive Strategy.
- Active monitoring of healthcare workers can be highly resource-intensive. There is limited evidence of increased effectiveness in prevention of nosocomial transmission beyond passive strategies.
- Acceptance by staff can be limited by perceptions of mistrust in ability to monitor and appropriately report symptoms.
- Active monitoring can decrease the likelihood that healthcare workers self-monitor signs and symptoms. Ideally, healthcare workers are checking their own temperature and symptoms and will not present if not indicated. Any action that weakens self-monitoring should be implemented with caution.
- To decrease workload, and if accountability can be maintained, the following can be delegated to unit/immediate supervisors (e.g., head/charge nurses, department heads):
- Responsibility for receiving symptom/temperature reports
- Monitoring staff compliance for the remote active strategy
6. Identification of Inpatients with suspected COVID-19
The development of acute respiratory infection and healthcare-associated pneumonia are common complications of hospitalization. However, it is important that clinicians maintain a high level of suspicion for COVID-19 when there is a compatible presentation. Because healthcare facilities often represent a gathering of individuals at higher risk of infection and adverse outcomes, the potential for outbreaks and harm to patients requires special effort to ensure any inpatient COVID-19 cases are identified.
A goal of identifying inpatients with suspected COVID-19 is to guide IPC strategies to prevent or limit transmission in healthcare setting. See interim WHO guidance on infection prevention and control during health care when COVID-19 is suspectedexternal icon.
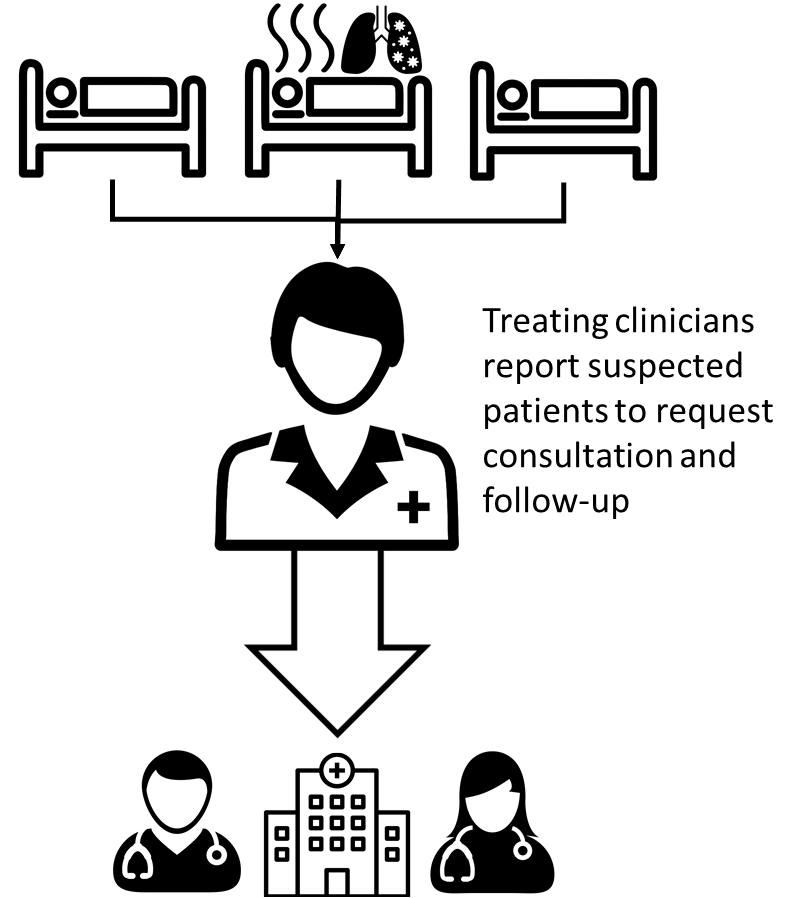
Figure: Passive strategy for identification of inpatients with suspected COVID-19
Passive Strategy:
Clinicians are kept informed6 on:
Clinicians are also made aware of what to do if they suspect COVID-19 in a hospitalized patient, including isolation precautions, PPE use, reporting/informing IPC focal point at the facility and public health authorities, and how to obtain testing, if available.
Recommended Surveillance Capacity Level:
Applicable at all HAI surveillance capacity levels (i.e., very low to high)
Rationale:
Minimal disruption of existing clinical practice and no requirement for standardized data collection or form completion. Strategy seeks to encourage recognition and reporting by astute clinicians.
Requirements:
- Regular and up-to-date educational materials/job aids provided to and accessible by clinicians
- COVID-19 case definitions
- Standard operating procedure (SOP) for response to identified suspect case patients (e.g., isolation, cohorting, PPE).
- Acceptable reporting/communication channels to hospital administration and public health authorities
Considerations:
- Strategy is dependent on participation and skill of available clinicians and an understanding of local epidemiology and clinical presentation of COVID-19, which may differ in different populations.
- Limited access to diagnostic testing will complicate this effort with the most conservative strategy being to treat all suspect cases as confirmed cases (empirical case determination) – potentially wasting resources, and if cases are cohorted, mixing positive and negative patients for extended periods.
- The degree of resource waste and case patient mixing will depend on the accuracy of empirical case determination.
- Supporting empirical case determination through clinician education and job aids (as described) can help improve accuracy of clinical diagnosis of COVID-19.
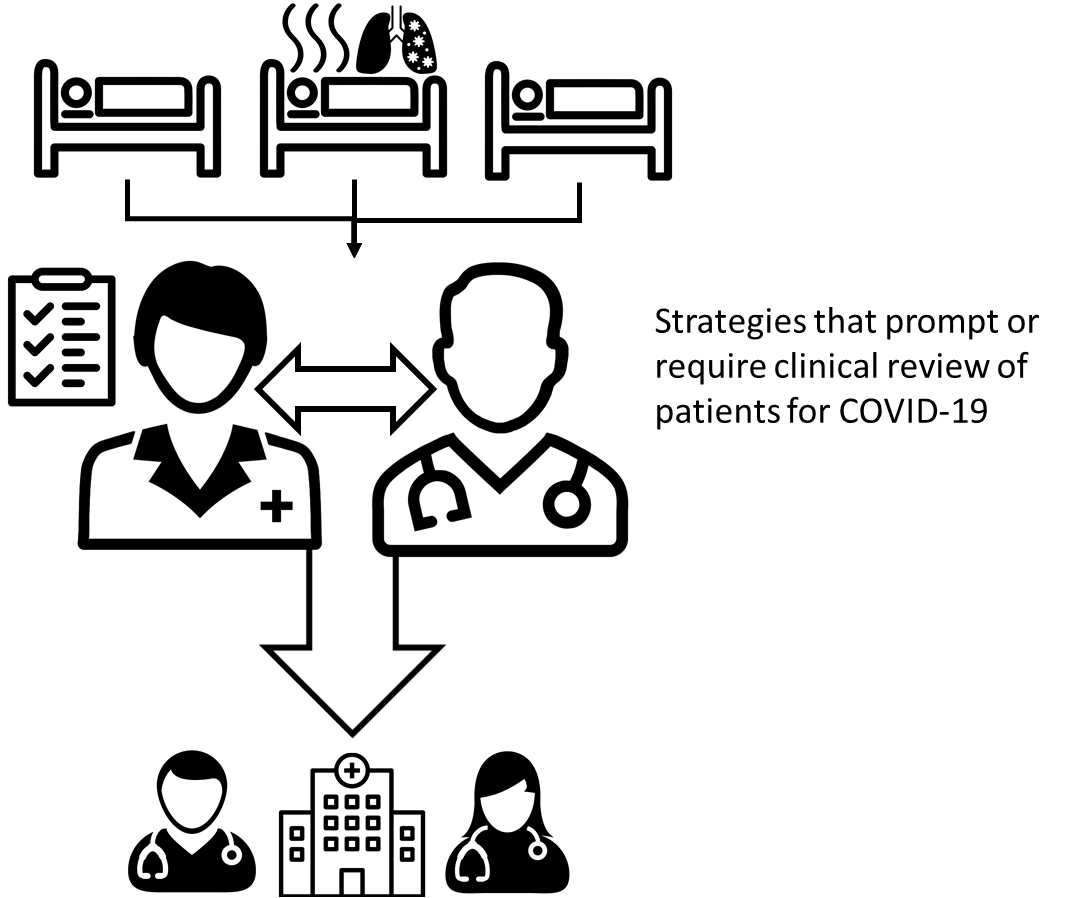
Figure: Enhanced passive strategy for identification of inpatients with suspected COVID-19
Enhanced Passive Strategy:
Enhancement of the passive strategy can be achieved through establishing systems that prompt or require clinicians to regularly review all patients for suspected COVID-19. Example enhanced passive strategies might include:
- Incorporating consideration of COVID-19 into sign-out reporting
- Requiring units to provide a daily clinician-generated list of suspected cases, including if there are zero cases
- Sending specific daily requests to clinicians to report and discuss encountered patients with symptoms consistent with COVID-19
Recommended Surveillance Capacity Level:
Applicable in most HAI surveillance capacity levels (very low to high)
Rationale:
Dialogue and accountability for case finding and reporting can improve empirical case determination, ensure patient evaluations are not missed, and help avoid clinician complacency over the long-term
Requirements:
- All requirements of Passive Strategy
- Strategy to prompt and/or ensure clinician review – requirements will depend on selected strategy
Considerations:
- Effective strategies will be context specific and require thought and effort in design and implementation
- May represent changes to current practice, which can limit acceptability
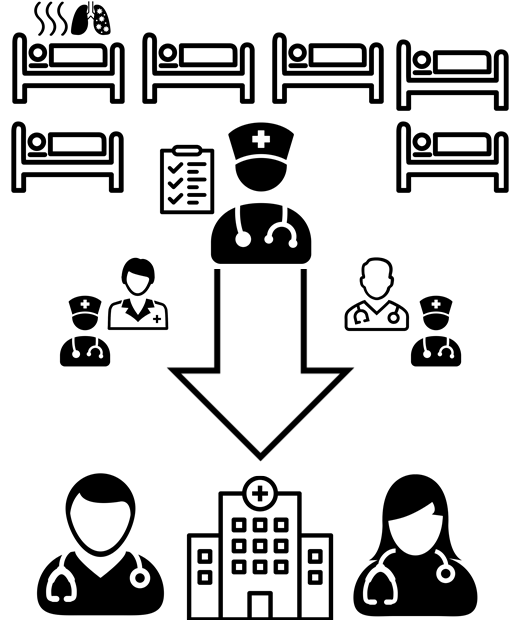
Figure: Active strategy for identification of inpatients with suspected COVID-19
Active Strategy:
Active case identification involves targeted data collection and review of patient information by groups specifically responsible for the identification of suspected COVID-19 cases. Examples of groups responsible for case identification and active case identification may include:
- Ministries of Health
- Sub-national/local public health authorities
- Facility infection prevention and control teams
Recommended Surveillance Capacity Level:
High existing surveillance capacity or medium capacity with the provision of additional resources
Rationale:
Smaller more centralized team responsible for case identification can increase overall quality through dedicated training, improved engagement, limiting of competing priorities, and standardization of methods
Requirements:
- Team with the information access, resources, and experience necessary for systematic review of patient information in order to appropriately apply standardized suspect case definitions
- Group(s) with availability and responsibility for data collection, analysis/presentation, and information sharing
- Group(s) with availability and responsibility for review of case-finding information with the authority and willingness to take appropriate action
Considerations:
- Highly resource-intensive
- Teams with the requisite skills can be difficult to build during outbreak response periods
- Separates case finding activities from patient care activities, which can decrease acceptability and impact sustainability
- Value of active inpatient case finding, especially the context of limited diagnostic testing, should be carefully considered